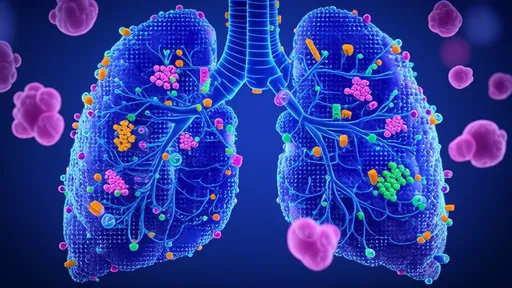
In the relentless battle against lung cancer, early detection remains a critical factor in improving patient outcomes. Traditional screening methods, such as low-dose computed tomography (LDCT), have proven effective but come with limitations, including cost, accessibility, and radiation exposure. Now, a groundbreaking approach using nanosensor arrays to analyze exhaled breath is emerging as a potential game-changer in early lung cancer detection.
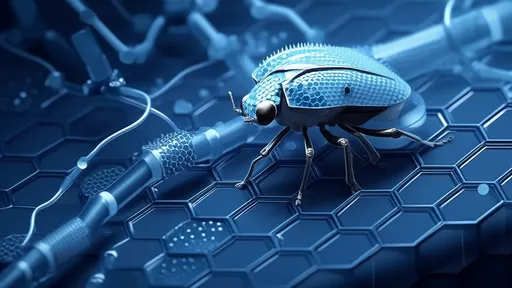
The science behind breath analysis for disease detection is not entirely new. For decades, researchers have explored the concept that specific volatile organic compounds (VOCs) in exhaled breath could serve as biomarkers for various diseases. However, recent advancements in nanotechnology and artificial intelligence have transformed this concept from theoretical possibility to clinical reality. Nanosensor arrays represent the cutting edge of this transformation, offering unprecedented sensitivity and specificity in detecting lung cancer at its earliest stages.
How Nanosensor Arrays Work
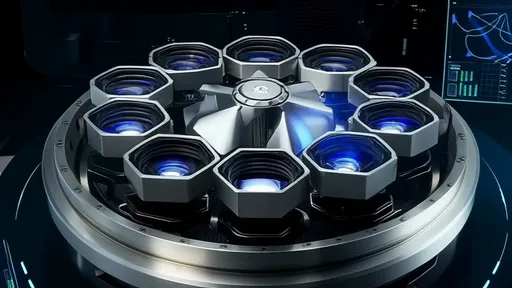
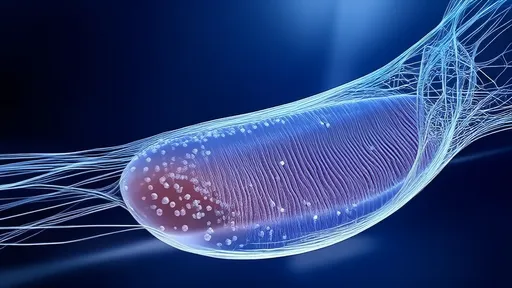
At the heart of this technology are sophisticated nanosensor arrays capable of detecting minute concentrations of cancer-associated VOCs in breath samples. These arrays typically consist of multiple sensors, each designed to respond to specific molecular patterns associated with lung cancer. When a patient exhales into the device, the sensors interact with the breath molecules, producing a unique response pattern that can be analyzed using machine learning algorithms.
The true innovation lies in the nanomaterials used in these sensors. Gold nanoparticles, carbon nanotubes, and metal-oxide semiconductors are among the materials being employed, each offering distinct advantages in terms of sensitivity and selectivity. Some systems use functionalized nanoparticles that change their electrical properties when they bind to specific cancer biomarkers, while others rely on changes in optical properties or mass.
Clinical Validation and Performance
Recent clinical studies have demonstrated the remarkable potential of nanosensor breath tests. In one notable trial involving hundreds of participants, a nanosensor array system achieved sensitivity and specificity rates comparable to LDCT, with the added advantage of being completely non-invasive. The technology has shown particular promise in distinguishing between benign pulmonary nodules and malignant ones - a critical challenge in current screening protocols.
Perhaps most impressively, some systems have demonstrated the ability to detect lung cancer at stage I with accuracy rates exceeding 85%. This early detection capability could dramatically improve survival rates, as stage I lung cancer has a five-year survival rate of about 55-70%, compared to just 5% for stage IV disease. The technology is also showing potential in detecting precancerous conditions, opening the possibility of intercepting the disease before it fully develops.
Advantages Over Current Screening Methods
The benefits of nanosensor-based breath testing are numerous. Unlike imaging-based methods, breath analysis requires no radiation exposure, making it safe for repeated use. The procedure is simple and quick, taking just minutes to complete, with no need for specialized facilities or highly trained personnel. This simplicity could dramatically increase screening participation rates, particularly in underserved populations where access to LDCT is limited.
Cost-effectiveness represents another significant advantage. While the initial development costs for nanosensor arrays are substantial, the per-test cost is expected to be significantly lower than LDCT, making large-scale screening programs more economically viable. Some estimates suggest breath testing could reduce screening costs by as much as 75%, while simultaneously increasing detection rates through improved patient compliance.
Challenges and Future Directions
Despite the promising results, several challenges remain before nanosensor breath testing can become a standard screening tool. Standardization of collection methods and analysis protocols is needed to ensure consistent results across different settings. The influence of confounding factors such as diet, smoking, and comorbidities on breath VOC profiles must be better understood and accounted for in the algorithms.
Researchers are also working to improve the technology's ability to distinguish between different types of lung cancer and to integrate it with other diagnostic modalities. The ultimate goal is to develop comprehensive breath-print databases that can not only detect lung cancer but also provide information about tumor characteristics, potentially guiding personalized treatment approaches.
The Road to Clinical Implementation
Several companies and research institutions are now advancing nanosensor breath tests through regulatory processes. Some systems have already received CE marking in Europe, while others are progressing through FDA clinical trials in the United States. The timeline for widespread clinical availability will depend on the outcomes of these trials and subsequent insurance coverage decisions.
As the technology matures, we may see breath-based screening integrated into routine health check-ups, particularly for high-risk individuals. Some envision a future where smartphone-connected breath analyzers enable frequent at-home screening, with AI-powered analysis providing instant risk assessments and recommendations for follow-up care.
The development of nanosensor arrays for lung cancer detection represents a convergence of nanotechnology, artificial intelligence, and clinical medicine that could transform how we approach cancer screening. While more research is needed, the potential to detect lung cancer earlier, more safely, and more cost-effectively offers hope for significantly reducing the global burden of this deadly disease.

By /Aug 14, 2025

By /Aug 14, 2025
By /Aug 14, 2025

By /Aug 14, 2025

By /Aug 14, 2025

By /Aug 14, 2025

By /Aug 14, 2025

By /Aug 14, 2025
By /Aug 14, 2025

By /Aug 14, 2025
By /Aug 14, 2025
By /Aug 14, 2025

By /Aug 14, 2025
By /Aug 14, 2025
By /Aug 14, 2025

By /Aug 14, 2025
By /Aug 14, 2025

By /Aug 14, 2025

By /Aug 14, 2025

By /Aug 14, 2025